
Precision Pain Relief
By the time a child is referred to the SickKids Chronic Pain Clinic, they’ve often lived with debilitating pain for months or even years. Persistent pain can disrupt life and derail childhood, and erode mental health and well-being. Though our pain teams teach coping strategies and offer physiotherapy, they also prescribe pain medications, varying the type and dose to find what’s most effective for their patients.
“We hear parents all the time asking about the safety of medications, and concerns about side-effects,” says Dr. Danielle Ruskin, Clinical and Health Psychologist at the SickKids Chronic Pain Clinic. They want to know: Will the drug even work? How will it interact with other medications? Will it cause side-effects? Unfortunately, standard prescription practices mean that we can only know the answers after a child has swallowed the pill.
But a powerful tool called pharmacogenomics could reveal potential problems before treatments are prescribed. And it has the potential to transform how doctors prescribe pain medication and other drugs in the future.
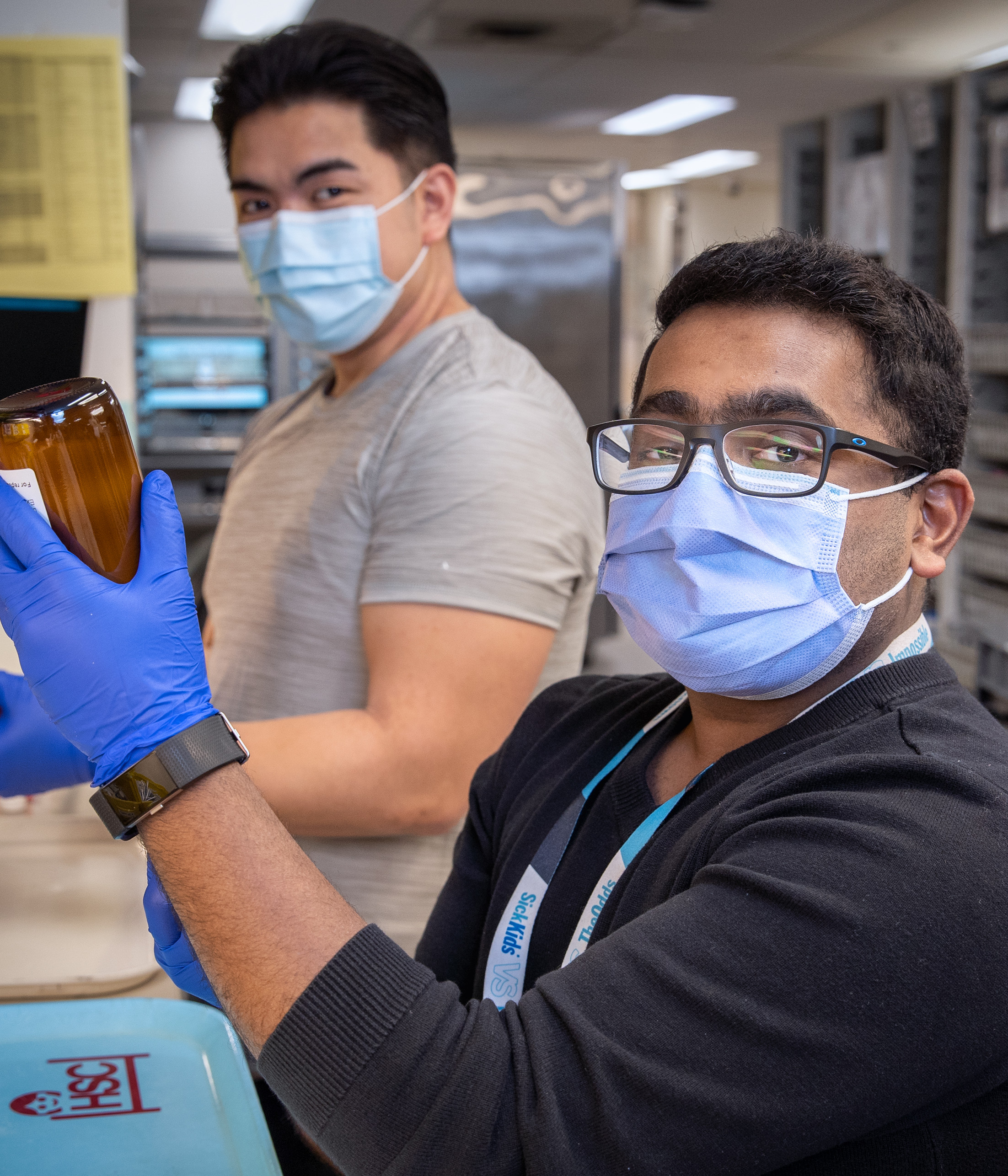
Pharmacogenomic testing analyzes a patient’s DNA to predict how they will respond to specific medications. At SickKids, Iris Cohn, a pharmacogenomic pharmacist — one of a handful in Canada — is working to integrate pharmacogenomic testing into clinical care. Since 2018, her team has used pharmacogenomic testing as a research tool to explain why a drug didn’t work for a patient, reasons for recurring side-effects, dosing issues, or to recommend an alternate drug. As part of this research, 450 SickKids patients have received pharmacogenomic testing for 65 medications.


Pharmacogenomic testing analyzes a patient’s DNA to predict how they will respond to specific medications. At SickKids, Iris Cohn, a pharmacogenomic pharmacist — one of a handful in Canada — is working to integrate pharmacogenomic testing into clinical care.
Most patients respond to medications as expected. But some patients are rapid or ultra-rapid metabolizers, which means they break the drug down too quickly and it has no effect. Others are slow metabolizers, so their body breaks down the drug too slowly, putting the patient at risk for serious side-effects.
To help bring pharmacogenomic testing into clinical use, Cohn is partnering with Ruskin to study how the practice could be used proactively to benefit patients and better inform the health-care providers who prescribe pain medications. Their research project received a Precision Child Health Catalyst Grant, made available thanks to generous donors to SickKids Foundation.
Over 18 months, the study of 50 patients (25 with chronic pain conditions and 25 preparing for major surgery) will track whether individualized prescribing leads to more rapid treatment responses and fewer side-effects, while hopefully giving patients and families greater confidence in the medications prescribed. In other words, the study would allow doctors to determine a patient’s best medicine before a single dose is administered. “Often parents feel helpless,” says Cohn. “Pharmacogenomics could empower them and give them peace of mind.”
Pharmacogenomics is a key pillar of our Precision Child Health initiative, which, alongside other applications of genome sequencing, big data and artificial intelligence, aims to treat patients based on what works for their unique genetics, environment and socioeconomics.
Precision Diagnostics
Last year, SickKids joined forces with three other top children’s hospitals to move the dial on childhood diseases.
The International Precision Child Health Partnership (IPCHiP) is an historic collaboration of SickKids, Boston’s Children’s Hospital (USA), Great Ormond Street Hospital (UK), and Murdoch Children’s Research Institute (Australia). Dr. Stephen Scherer, Chief of Research at SickKids, has been a driving force behind this partnership, which aims to pool genomics expertise, advance data science and AI, and ultimately, accelerate how paediatric diseases are diagnosed and treated.
In what’s thought to be the first global collaboration on Precision Child Health, IPCHiP will decode complex genetics of various paediatric diseases. Their first clinical research project looks at early-onset epilepsy that remains unexplained after standard testing. Using rapid whole-genome sequencing, their goal is to cut diagnosis time from three months to less than three weeks. The study has the potential to transform lives for babies with epilepsy. But the bigger goal is to establish a model that can be used to rapidly diagnose and treat other childhood diseases.